New state-level data reveal that syphilis cases continue to rise among gay and bisexual men in the US, with men in the south having the highest rates, according to a presentation at the 2016 STD Prevention Conference last week in Atlanta. A related study found that half of gay and bisexual men in 20 US cities were screened for syphilis during the past year, with 11% testing positive.
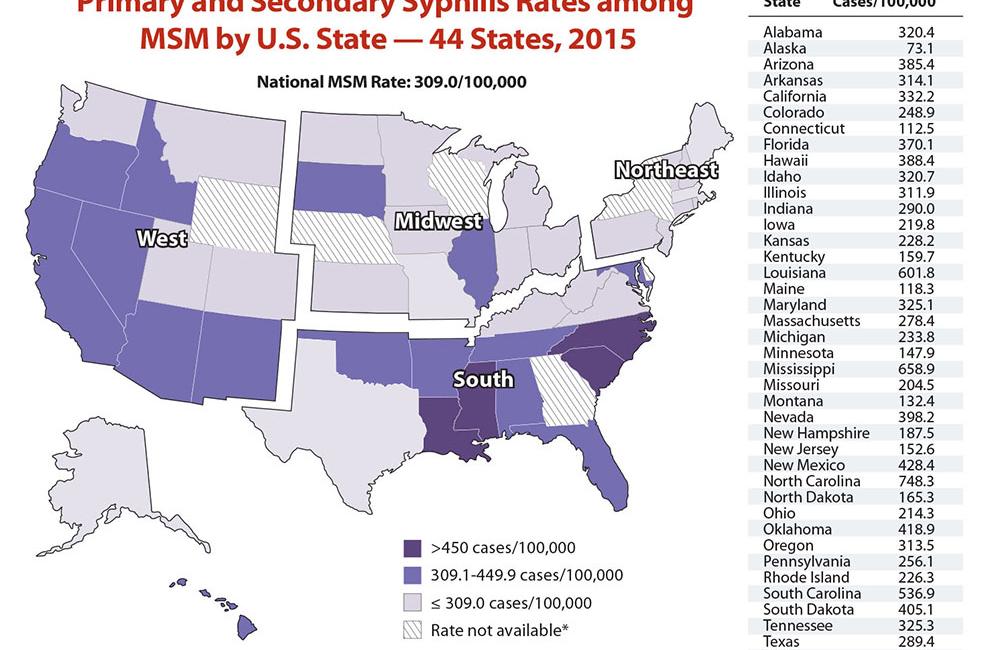
Alex de Voux of the US Centers for Disease Control and Prevention (CDC) and colleagues calculated the first-ever state-level estimates of primary and secondary syphilis rates among men who have sex with men (MSM).
Syphilis rates have been rising in the US in recent years. During 2014 there were more than 63,000 reported new cases of syphilis, including 20,000 cases of primary and secondary syphilis, with more than 80% of the latter occurring among MSM, according to the CDC. Reported syphilis cases rose by 15% from 2013 to 2014 and another 19% from 2014 to 2015, Dr de Voux said.
Primary syphilis, or initial infection, is marked by a single chancre or lesion in the genital or anal region where Treponema pallidum bacteria enter the body. These sores are typically painless, heal on their own and may never be noticed. If left untreated the infection progresses to the secondary stage, characterised by a rash on the mucous membranes and skin, including the palms and soles of the feet, sometimes accompanied by fever, swollen lymph nodes, fatigue and other flu-like symptoms.
These symptoms also go away without treatment, but the bacteria remain in the body and untreated infection progresses to the latent stage, which can last for years without symptoms. A minority of infected people go on to develop late-stage syphilis, which can involve damage to the heart, eyes (ocular syphilis), nervous system (neurosyphilis) and other organs. Pregnant women with syphilis can pass it to their babies (congenital syphilis).
Dr de Voux's team based their estimates on 2015 national syphilis case report data from the National Notifiable Diseases Surveillance System, along with 2014 estimates of the number of adult gay and bi men by state. State-level estimates of syphilis among gay men were not previously possible because state-by-state estimates of this population were not available, they noted. This missing denominator was provided by recent estimates of the number of MSM in each state from researchers at Emory University.
The CDC researchers calculated rates for the 44 states that reported the sex of partners for at least 70% of men diagnosed with primary and secondary syphilis during 2015 – which accounted for 84% of all such cases – comparing rates among men with any male partners versus those reporting only female partners.
Nationwide there were 17,887 cases of primary and secondary syphilis among all men and 2030 cases among women in these 44 states in 2015. Among men, the case numbers were 12,118 for MSM, 2866 for heterosexual men and 2903 for men with unknown sex of partners.
The nationwide syphilis rate among gay and bi men in 2015 was 309.0 cases per 100,000, compared with 2.9 per 100,000 among heterosexual men. Although there were about four times as many cases of syphilis among MSM compared to heterosexuals, when taking into account their much smaller number in the population the rate was 107 times higher.
Alaska had the lowest rate of primary and secondary syphilis among MSM (73.1 per 100,000), while North Carolina had the highest rate (748.3 per 100,000). Three other states in the southeast also had among the highest rates in the nation: Mississippi (658.9 per 100,000), Louisiana (601.8 per 100,000) and South Carolina (536.9 per 100,000).
Syphilis testing and diagnosis trends
In a related analysis Cyprian Wejnert, also from the CDC, and colleagues looked at trends in syphilis screening and diagnosis among gay and bi men.
The CDC recommends that all sexually active men who have sex with men should receive routine annual screening for syphilis, while those at increased risk should be tested every three to six months.
This study looked at National HIV Behavioral Surveillance data for sexually active adult MSM in 20 US cities in 2008, 2011 and 2014. The analysis included data from more than 30,000 gay and bi men overall, including more than 10,000 in 2014.
Participants self-reported their sexual and drug-related risk and prevention behaviours, including whether they received HIV, hepatitis C and sexually transmitted infection screening during the previous 12 months.
Overall, nearly half of men (49%) surveyed in 2014 said they had been tested for syphilis within the past 12 months, up from 38% in 2008 and 40% in 2011.
Rates of syphilis screening in 2014 were similar across racial/ethnic groups, at 50% for black men and 48% for both white and Latino men. Men who had seen a healthcare provider in the past year were more likely to have been screened than those who had not (54 vs 25%), and those with insurance were more likely than those without (51 vs 42%).
Gay and bi men at highest risk were most likely to be tested for syphilis, including HIV-positive men (68 vs 45% of HIV-negative) and men with more than 10 sexual partners during the past 12 months (65 vs 45% among those with fewer partners).
Among sexually active men who were screened, the proportion who tested positive for syphilis was 11% in 2014, up from 9% in 2008 and 8% in 2011. Although black men were only slightly more likely to be screened, they had a substantially higher rate of syphilis diagnosis (14%) than white (8%) or Latino (11%) men in 2014.
HIV-positive men were nearly three times more likely to have syphilis than HIV-negative men (21 vs 8%), and men with more than 10 sexual partners were about twice as likely as those with fewer partners (17 vs 9%).
The largest increases in syphilis diagnoses were seen among black MSM (rising from 9% in 2008 to 14% in 2014), HIV-positive men (15 to 21%), men with 10 or more sexual partners (11 to 17%) and young men (from 6 to 10%).
"Despite the recommendation for at least annual screening among all sexually active MSM, less than one-half of MSM reported recent syphilis screening in 2014," the researchers concluded in their abstract. "While screening among MSM increased, more work is needed, especially given increases in syphilis diagnosis among those screened from 2008 to 2014."
Ocular syphilis
Finally, Anna Cope and Sara Oliver, both from the CDC, presented new data on ocular syphilis, an uncommon but serious manifestation.
Although syphilis rates have been increasing nationwide since 2000, ocular syphilis clusters have only been reported since late 2014, Dr Oliver noted. Between December 2014 and March 2015 a dozen cases of ocular syphilis were reported in San Francisco and Seattle, and subsequent case finding identified more than 200 cases in 20 states reported over the past 2 years, according to the CDC.
Dr Oliver and colleagues sought to systematically identify ocular syphilis cases in North Carolina, determine associated risk factors and compare syphilis cases with and without ocular manifestations.
Among 4234 syphilis patients identified during 2014-2015, a total of 63 (1.5%) had ocular syphilis. There were 20 cases in 2014 and 43 cases in 2015 – a 115% increase in ocular syphilis, even though syphilis cases overall increased by just 35%.
All but four ocular syphilis cases were in men, and 71% of these were MSM. Patients with ocular syphilis presented at all stages of disease, including 24 (38%) during primary or secondary syphilis. Individuals with ocular manifestations were more likely to be age 40 or older and HIV-positive. No behavioural risk factors were associated with ocular syphilis.
Dr Cope's report focused on the association between ocular syphilis and HIV status. Of the total 4232 people with syphilis, 1694 (40%) were HIV positive, but they accounted for 35 (56%) of the 63 ocular syphilis cases.
Ocular syphilis was 90% more prevalent among HIV-positive compared to HIV-negative people or those of unknown HIV status. Among HIV-positive people diagnosed with syphilis, those concurrently diagnosed with ocular syphilis were older (48 vs 27 years), had a higher median HIV viral load and were more likely to be in the latent stage of syphilis. Ocular syphilis was also associated with lower CD4 cell counts.
“The association between older age, lower CD4 counts and ocular syphilis prevalence suggests immune status may play a role in ocular syphilis development and highlights the importance of HIV screening in all syphilis patients, especially those with ocular syphilis,” the researchers concluded.
These findings support the CDC’s recommendation that clinicians should consider testing for HIV if they see a patient with ocular syphilis, issued earlier this year after the outbreaks in San Francisco and Seattle.
Taken together, these studies underscore the importance of syphilis screening and follow-up care for gay and bisexual men, as prompt diagnosis and complete antibiotic treatment can both prevent long-term health complications and interrupt onward transmission.
de Voux A et al. Rates of Primary and secondary syphilis by state among men who have sex with men – United States, 2015. 2016 STD Conference, Atlanta, abstract 4B1, 2016. View abstract.
Wejnert C et al. Syphilis screening and diagnosis among men who have sex with men, 2008-2014, 20 U.S. cities. 2016 STD Conference, Atlanta, abstract 4B4, 2016. View abstract.
Oliver S Increase in ocular syphilis – North Carolina, 2014-2015. 2016 STD Conference, Atlanta, abstract 4B2, 2016. View abstract.
Cope A et al. Ocular syphilis and HIV coinfection: an opportunity to identify previously undetected HIV. 2016 STD Conference, Atlanta, abstract 3F1, 2016. View abstract.
