HIV raises the risk of death from COVID-19 in South Africa’s Western Cape province and around eight percent of deaths from COVID-19 in the province are attributable to HIV, Dr Mary-Ann Davies of the Western Cape Health Department told the 23rd International AIDS Conference (AIDS 2020: Virtual) today.
However, the increase in risk is modest and although HIV prevalence in South Africa is high, the relative youth of the population living with HIV means that the absolute number of deaths due to HIV remains small.
The analysis looked at approximately 3.5 million adults receiving public sector health care in the Western Cape province, both in the community and in hospital. Most other studies on COVID-19 in people with HIV have only included hospitalised patients. The analysis investigated risk factors for death in people with a positive SARS-CoV-2 test, providing updated data and more detailed analyses than a previous presentation of the findings. The study methodology was described in our report on that presentation.
There was a total of 22,308 diagnosed cases of SARS-CoV-2, including 625 deaths.
People who died were substantially older than other people with diagnosed COVID-19 or than people in the wider population (63 years vs 37 and 38 years respectively). People who died also had a higher prevalence of diabetes, hypertension, chronic kidney disease, chronic obstructive pulmonary disease, and previous or current TB.
HIV prevalence was similar across the three groups at around 17%. However, there were several differences in the characteristics of HIV-positive and HIV-negative people who died. Nearly three-quarters of people living with HIV who died (74%) were under the age of 60 compared to 37% of HIV-negative people. People living with HIV were much more likely to have had a previous (37%) or current (14%) tuberculosis infection compared to HIV-negative people (9%, 2%).
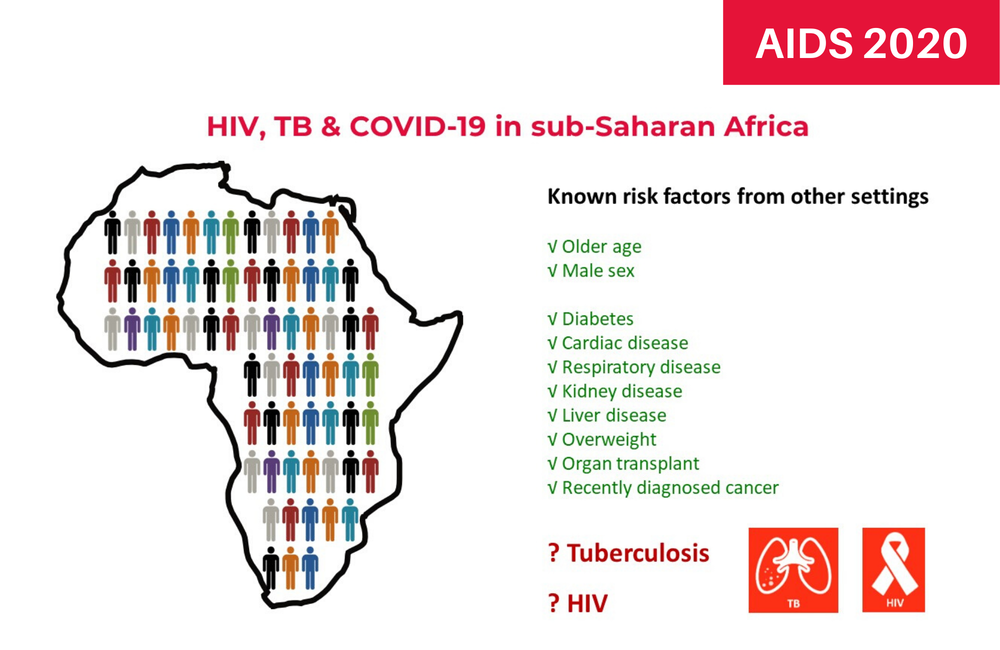
The strongest risk factors for COVID-19 death in the Western Cape population were older age and diabetes. Tuberculosis and HIV were also risk factors, but to a lesser extent.
Compared with people aged 20-39 years, who had a death rate of 24 per million from COVID-19 in the first 100 days of the pandemic in Western Cape, the risk of death increased in each age stratum, so that people aged 60-69 were eleven times more likely to die of COVID-19 than the younger age group (adjusted HR 11.54,95% CI 8.11-16.42) and the over-70s were more than 16 times more likely to die (aHR 16.79 [11.69-24.11]).
Diabetes raised the risk of death between five- and twelve-fold depending on the extent to which blood sugar was controlled. Other co-morbidities did not increase the risk of death to the same extent. Hypertension had a modest effect on the risk of death (aHR 1.31 [1.09-1.57]) and chronic kidney disease also raised the risk of death (aHR 1.86 [1.49-2.33]) but chronic obstructive pulmonary disease and asthma were not associated with an increased risk of death.
Current tuberculosis more than doubled the risk of death (aHR 2.71 [1.81-4.04]) while a past TB diagnosis increased the risk of death by around 50% (aHR 1.51 [1.18-1.93]).
HIV infection doubled the risk of death (aHR 2.14 [1.70-2.70]). After taking into account the expected number of COVID-19 deaths based on the age and sex profile of the HIV-positive population, investigators calculated that the standardised mortality ratio (the increase in deaths) for people with HIV was 2.39 (95% CI 1.96-2.86). Approximately 8% of COVID-19 deaths could be attributed to HIV, they calculated.
Comparing people with HIV by immune status and viral suppression, the investigators found that people with HIV who had a viral load above 1000 or a CD4 count below 200 (the 'not well' group) had a somewhat higher risk of death (aHR 3.35 [1.83-6.12]) than people with suppressed viral load and recent antiretroviral therapy (aHR 2.61 [1.98-3.43]).
The presence of tenofovir (TDF) in the antiretroviral regimen was associated with a reduced risk of COVID-19 death (aHR 0.42 [0.22-0.78]) after controlling for kidney disease and viral suppression but Davies cautioned that this finding is hard to interpret.
Davies stressed that the increased risk of COVID-19 death in people with HIV is modest and may be an over-estimate if residual confounding factors (such as socioeconomic status and co-morbidities) have been missed.
Davies MA et al. Western Cape: COVID-19 and HIV / Tuberculosis. 23rd International AIDS Conference, abstract OAXLB0106, 2020.
Update: Following the conference presentation, this study was published in a peer-reviewed journal:
Boulle A et al. Risk factors for COVID-19 death in a population cohort study from the Western Cape Province, South Africa. Clinical Infectious Diseases, online ahead of print, August 2020.
DOI: 10.1093/cid/ciaa1198
