A man in São Paulo who has no evidence of remaining HIV after more than 15 months off antiretrovirals – at least according to tests done so far – may represent the first case of a functional cure without the risks of a stem cell transplant, according to a report presented today at the 23rd International AIDS Conference (AIDS 2020: Virtual).
As part of a clinical trial, the 35-year-old man had two additional antiretrovirals, the integrase inhibitor dolutegravir (Tivicay) and the entry inhibitor maraviroc (Celsentri), added to his standard three-drug regimen. In addition, he received nicotinamide, a water-soluble form of niacin, or vitamin B3.
He underwent a closely monitored treatment interruption in March 2019. More than 15 months later, he continues to have undetectable HIV RNA (the form of viral genetic material measured in a typical viral load test) as well as undetectable HIV DNA (the form that largely makes up the viral reservoir).
But experts caution against reading too much into this case, as it involved only a single individual and extensive testing for traces of HIV at various sites in the man's body have not yet been carried out.
"The fact that it's a single case suggests that this may not be real," Dr Steven Deeks of the University of California in San Francisco told aidsmap. "We know that some people can achieve what appears to be remission with antiretroviral drugs alone. This may simply be a person who got lucky with antiretrovirals."
An easier way to remission?
So far, two people appear to have been cured of HIV. Timothy Ray Brown, formerly known as the Berlin Patient, has had no evidence of replication-competent HIV anywhere in his body for more than 13 years. The second man, dubbed the London Patient, still has no detectable virus as he approaches three years off antiretroviral therapy (ART).
Both men received bone marrow transplants to treat leukaemia or lymphoma using stem cells from a donor with a rare genetic mutation known as CCR5-delta-32, which results in missing CCR5 co-receptors on T cells, the gateway most types of HIV use to infect cells. Before the transplants, they received chemotherapy to kill off their cancerous immune cells, essentially allowing the donor stem cells to rebuild a new HIV-resistant immune system.
But this procedure is far too dangerous for people whose lives are not already threatened by advanced cancer. What's more, it requires intensive medical intervention, is extremely expensive and could probably not be scaled up enough to make it feasible for the millions of people living with HIV worldwide.
This has led researchers to ask whether the right combination of medications could offer a safer and less expensive path to long-term remission – or ultimately a cure.
Dr Ricardo Diaz of the University of São Paulo in Brazil, Dr Andrea Savarino of the Italian Institute of Health in Rome and their team conducted a clinical trial known as SPARC-7 to evaluate multiple interventions aimed at reducing the size of the HIV reservoir.
This reservoir is comprised of latent HIV integrated into inactive host cells, primarily T cells. Antiretrovirals cannot reach this hidden virus, but if treatment stops and the cells become reactivated, they can once again begin churning out new copies of the virus.
The study enrolled HIV-positive adults who were on their first antiretroviral regimen, had viral suppression for more than two years and had never had a CD4 count below 350 cells/mm3.
Five of the participants added dolutegravir, maraviroc and 500mg twice daily of nicotinamide to their original three-drug antiretroviral regimen for 48 weeks. They then reverted back to standard ART and finally underwent an analytical treatment interruption, in which viral load and other parameters are closely monitored.
As Savarino explained in an interview with aidsmap prior to the conference (watch above), nicotinamide was chosen because it appears to fight HIV by multiple mechanisms. Available as an inexpensive oral supplement, nicotinamide is being studied as a cancer treatment because of its immune-boosting properties. It helps prevent exhausted T cells from committing suicide (apoptosis) by inhibiting the activity of enzymes called PARPs that repair broken DNA. It may also act as a histone deacetylase (HDAC) inhibitor that keeps T cells out of a latent state. Maraviroc, too, may act as a latency-reversing agent in addition to its better-known effect of blocking HIV entry into cells.
One individual remains in remission
The Brazilian who remains in remission was diagnosed with HIV in October 2012, at which time he had a lowest-ever CD4 cell count (372 cells/mm3) and viral load (over 20,000 copies/ml) characteristic of chronic infection. Two months later, he started treatment with efavirenz (Sustiva), zidovudine (AZT) and lamivudine (3TC), substituting tenofovir disoproxil fumarate (TDF) for zidovudine in 2014.
The man enrolled in the clinical trial in September 2015 and started on the intensified ART regimen plus nicotinamide. Among the 30 participants receiving various investigational regimens in the study, he was the only one who experienced low-level viral blips during his experimental treatment (at weeks 16 and 24), but his viral load thereafter remained undetectable.
After completing 48 weeks on this combination, he returned to his prior three-drug regimen, later swapping out efavirenz for nevirapine (Viramune) and ultimately dolutegravir. Throughout, he maintained viral suppression.
In March 2019, he started an analytical treatment interruption, stopping his antiretroviral therapy under medical supervision. Today, his viral load remains undetectable according to HIV RNA blood tests done every three weeks. His last test was on 22 June 2020, meaning he has maintained viral suppression for more than 65 weeks off antiretrovirals.
The man's CD4 cells were generally stable while on the experimental intensified regimen, rose after returning to standard three-drug therapy and then dropped after starting the treatment interruption.
Various markers of CD8 cell activation – the type of T cells that fight HIV – declined after starting the intensified regimen and remained below the baseline level.
Looking at other parameters can give clues about whether HIV remains present but under control or has truly been eliminated.
The man's HIV DNA level in peripheral blood immune cells rose after starting the experimental regimen – suggesting the treatment may have reactivated latent reservoir cells – but then fell to an undetectable level after he resumed standard ART. It has remained undetectable during the treatment interruption.
HIV DNA in the man's gut biopsy samples declined while he was on the intensified regimen. Further analysis of HIV in gut tissue, lymph nodes and other sites – as Timothy Brown has undergone – will be needed to show whether the man is in fact functionally cured. However, Savarino told aidsmap that these more invasive tests have been put on hold due to COVID-19 restrictions on health services in Brazil.
"Four other individuals treated with the same intensified regimen did not maintain viral suppression."
The presence of HIV antibodies indicates that, even while on treatment, enough of the virus remains to stimulate ongoing antibody production. In this case, the man's antibody level declined steadily while he was on the experimental regimen and continued to fall after he resumed three-drug therapy. During the treatment interruption, he maintained a very low antibody level – low enough that a rapid antibody test became negative.
Importantly, Savarino told aidsmap, four other individuals treated with the same intensified regimen did not maintain viral suppression.
Speaking at a media briefing, conference co-chair Dr Anton Pozniak of Chelsea and Westminster Hospital recalled that we have heard of many other potential HIV cures before – including the famed Mississippi baby, who maintained viral suppression off antiretrovirals for more than two years before her virus rebounded – but so far these have mostly ended in disappointment.
Deeks urged caution about "overinterpreting" the findings from this case, which does not suggest any interventions that people living with HIV should undertake on their own at this time. In particular, people should not start taking nicotinamide or niacin, which can cause an uncomfortable flushing side effect at high doses.
"I would certainly encourage people to not jump on this. This may not be real and it could actually cause harm," he said. "I would not encourage anyone to run out to the local health food store and get this drug, and don’t stop taking antiretrovirals."
Diaz RK et al. The first long-term remission of chronic HIV-1 infection without myeloablation? 23rd International AIDS Conference, abstract OAXLB0105, 2020.
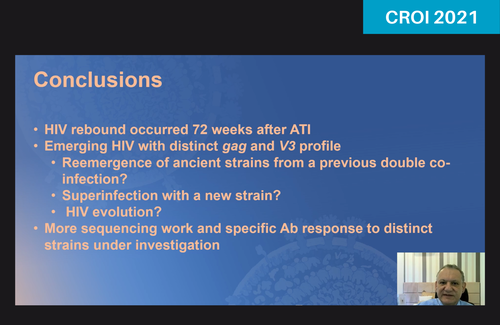
An update on this case was presented at CROI 2021: São Paulo patient experiences apparent viral rebound a year and a half after stopping HIV treatment.