PrEP implant could last well over a year

Dr Randolph Matthews of Merck. Photo by Liz Highleyman.
An implant containing a new antiretroviral could provide sustained levels of drug sufficient to prevent HIV infection for over a year, Dr Randolph Matthews told the 10th International AIDS Society Conference on HIV Science (IAS 2019) in Mexico City.
The drug, islatravir, formerly known as MK-8591, is a nucleoside reverse transcriptase translocation inhibitor (NRTTI) with an extremely long half-life, meaning it is well-suited to long-acting formulations. Oral islatravir is also under investigation as an HIV treatment.
Merck, the company which developed the drug, has begun work to test its potential as pre-exposure prophylaxis (PrEP). It formulated islatravir as an implant, a small plastic insert that is placed under the skin of the upper arm.
The study of the PrEP implant announced at the conference evaluated levels of the drug (versus placebo) in two different doses (54mg and 62mg per implant) given to 16 individuals for a three-month period. The purpose of the study was to assess safety and tolerability, and to estimate the time at which the concentration of islatravir would fall below the minimum effective level to stop HIV replication.
The 62mg dose produced levels above this threshold in all trial volunteers for the three months the implant was in place, whereas levels fell below this for part of the time in a few people given the lower dose.
Although this was only a three-month study, projections show that the concentration of the drug produced by the implant should stay well above the prevention threshold for at least a year, and probably considerably longer.
Dolutegravir leads to weight gain in two African studies
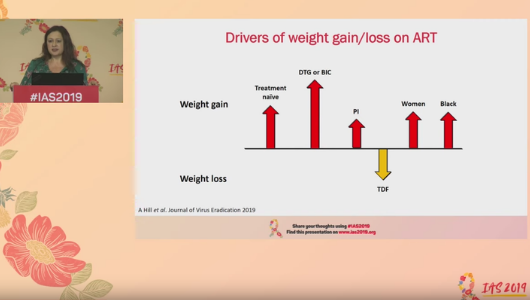
Image from the livestream of Michelle Moorhouse presenting at IAS 2019.
The NAMSAL trial randomised 613 adults in Cameroon to either the older formulation of tenofovir (tenofovir disoproxil fumarate – TDF), lamivudine and dolutegravir or tenofovir, lamivudine and efavirenz. Participant body weight was measured at baseline and at week 48. After 48 weeks, participants in the dolutegravir arm of the study had gained a median of 5kg compared with a 3kg gain in the efavirenz arm. Weight gain of greater than 10% of body mass was significantly more likely to occur in women taking dolutegravir when compared to efavirenz, but there was no significant difference in weight gain by regimen in men.
The ADVANCE study randomised 1053 adults and adolescents in South Africa to either tenofovir (TDF), emtricitabine and dolutegravir; the new formulation of tenofovir (tenofovir alafenamide fumarate – TAF), emtricitabine and dolutegravir; or tenofovir (TDF), emtricitabine and efavirenz. After 48 and 96 weeks, weight gain was greatest in the group taking TAF/emtricitabine/dolutegravir. Weight gain was lower in the TDF/emtricitabine/dolutegravir group and lowest in the TDF/emtricitabine/efavirenz group.
In the ADVANCE study, there was also a significant difference in weight gain by gender. Men and women randomised to dolutegravir gained weight to a similar extent up to week 48, but whereas male weight stabilised after week 48, women continued to gain weight.
Longer-term follow-up is needed to evaluate the consequences of weight gain in these study populations. Moorhouse said that analysis of other trial populations is needed to look at weight gain in different settings and populations.
WHO endorses event-driven PrEP for gay men

Jean-Michel Molina at IAS 2019. Photo by Liz Highleyman.
The World Health Organization (WHO) has updated its recommendation for pre-exposure prophylaxis (PrEP) to include event-driven PrEP taken before and after sex as an HIV prevention option for men who have sex with men. The update was announced this week at IAS 2019.
The conference featured numerous presentations on PrEP, including a report that no participants in the French Prévenir study who consistently used either daily or event-driven PrEP have acquired HIV.
Event-driven PrEP – also called on-demand PrEP or the 2+1+1 schedule – involves taking a double dose (two pills) of Truvada (tenofovir disoproxil fumarate/emtricitabine) between 2 and 24 hours before sex is anticipated, and then, if sex occurs, one pill 24 hours after the double dose and another 24 hours later. If sex occurs several days in a row, one pill should be taken each day, until 48 hours after the last event.
In 2015, Dr Jean-Michel Molina of the University of Paris reported that event-driven PrEP reduced the risk of HIV infection by 86% among gay and bisexual men in the French Ipergay study – equalling the protective effect of daily PrEP in the UK PROUD study.
Following Ipergay, Molina's group embarked on the Prévenir study. Study participants could opt to take Truvada either daily or according to the event-driven schedule. As of early May 2019, Prévenir had enrolled 3057 men at 26 sites. About half the men opted for event-driven PrEP. Two men have seroconverted during follow-up, both in the event-driven PrEP group. However, both had stopped taking PrEP several weeks before and had condomless sex in the interim.
In 2015, WHO recommended that oral PrEP "should be offered as an additional prevention choice for people at substantial risk of HIV infection as part of a combination prevention approach," but did not endorse the event-driven regimen.
The update says that event-driven PrEP dosing is an option for men who have sex with men. This regimen is appropriate for men who would find intermittent PrEP more effective and convenient, those who have sex less frequently and those who can plan for sex at least two hours in advance.
Event-driven PrEP is not recommended for cisgender or transgender women, transgender men who have vaginal/frontal sex or men having sex with women. Additional research is needed into alternative regimens, taking into account the different pharmacology of tenofovir in the female genital tract. The regimen is also not suitable for people with chronic hepatitis B.
Men accounted for two-thirds of HIV transmission in PopART prevention trial

William Probert at IAS 2019. Photo by Roger Pebody.
PopART was a cluster-randomised trial of the impact of a universal test-and-treat strategy on HIV incidence. The trial took place in communities in Zambia and KwaZulu-Natal, South Africa. Communities were randomised to receive standard HIV testing and treatment services or to receive door-to-door testing and linkage to HIV care, with immediate treatment.
HIV incidence fell by 30% in the communities receiving testing at home and immediate treatment, compared to those receiving routine standard-of-care services.
Investigators wanted to know whether any groups of people were more likely to pass on HIV in this study, as a result of not being on treatment, being disengaged from care or experiencing treatment failure.
After analysing the genetic profile of viruses acquired by participants in the study, the researchers found that the groups most likely to pass on HIV were men between the ages of 25 and 29, and women between the ages of 20 and 24.
Two-thirds of all transmissions were estimated to have been from men to women, emphasising the importance of engaging young men in care and ensuring that they can maintain undetectable viral load.
South Africa saves $326 million on dolutegravir
South Africa’s public sector will save US$326 million over the next three years as a result of a competitive tendering exercise that pushed the price of a fixed combination of tenofovir, lamivudine and dolutegravir down to $65 per person, per year. The savings will help South Africa to treat around 2 million extra people, Herbert Musariri of the Clinton Health Access Initiative told IAS 2019.
South Africa has the largest HIV treatment programme in the world. Over 4.7 million people are already receiving antiretroviral treatment, largely through the public sector, making the South African government the largest procurer of antiretroviral drugs in the world.
The government has steadily driven down the cost of antiretroviral treatment through tendering exercises. Its most recent exercise, in 2018, set a maximum price for the first time. Eight suppliers were selected, including three in South Africa, to promote security of supply and reduce the risk of drug stock-outs.
Musariri said South Africa’s experience could help other countries to negotiate lower prices too.
Low harm reduction coverage for people who inject drugs in South Africa

Image from Andrew Scheibe’s presentation slides at IAS 2019. Original image source: TB HIV Care 2018
South Africa is part of numerous trading routes of drugs that are injected and injecting drug use has risen over the last two decades. Between 14 and 21% of the estimated 75,000 people who inject drugs in South Africa are living with HIV.
The World Health Organization (WHO) recommends harm reduction services for people who inject drugs should include: needle and syringe programmes (providing 300 needles per person, per year); opioid substitution therapy (with coverage of at least 40%); HIV testing and counselling; and that all people diagnosed with HIV start HIV treatment.
Scheibe used programme data from January to June 2018 to assess needle distribution, opioid substitution therapy coverage and the HIV treatment cascade among people who inject drugs who were accessing harm reduction services in the five cities.
Needle and syringe services distributed an average of 76 needles per person using the service per year, ranging from 52 per person in Pretoria to 174 in Cape Town. Only 260 people were on opioid substitution therapy, representing only 4% coverage across the cities (from 0% in Port Elizabeth to 8% in Cape Town).
In total, only 24% of people accessing the services were tested for HIV over the period. Of those tested, an average of 23% were diagnosed with HIV and only 20% of those diagnosed started antiretroviral therapy.
The researchers concluded that needle distribution needs to double, opioid substitution therapy coverage needs to expand tenfold, and access to HIV testing and treatment needs to increase fivefold.
Home tests aren’t an accurate way for people on HIV treatment to check they still have HIV

Testing programmes report significant numbers of people who have already been diagnosed re-testing, sometimes as part of a process of re-engaging with care but often because of doubts about the initial diagnosis. In the South African context, there are significant numbers of bogus practitioners who claim to cure individuals. With increasing discussion of ‘undetectable = untransmittable’, an emerging reason is due to misunderstanding of the nature of an undetectable viral load.
As self-testing programmes scale up, there are more opportunities for people to test, but without any interaction with healthcare professionals who might be able to explain the meaning of a result or arrange follow-up testing. The danger is that people who want to confirm their HIV status get an indeterminate or non-reactive result (i.e. a false negative) or low-reactive (indeterminate) result and stop taking their antiretroviral therapy.
In this study, samples from 100 people with HIV were tested with one oral fluid-based and five blood-based rapid diagnostic tests. The results were read and interpreted by two nurses.
Nine participants had at least one non-reactive result on at least one assay. Several participants had non-reactive (false negative) results on multiple tests. Of all 600 tests performed, there were 16 non-reactive results as well as 74 low-reactive results.
Dr Mohammed Majam, who presented the study, concluded that false negative results have serious implications for HIV self-testing programmes.
Scientific analysis from Clinical Care Options

Clinical Care Options is the official provider of online scientific analysis for IAS 2019 through capsule summaries, downloadable slides, rapid expert webinars, and ClinicalThought commentaries.
