Healthcare workers caring for people living with HIV are expressing concern over those who are not virally suppressed, late presenters and how to manage new HIV diagnoses during the global COVID-19 pandemic. There are also concerns about access to medication and increased vulnerabilities of key populations.
Leading HIV clinicians from around the world gave insight into HIV service provision during the COVID-19 pandemic at two International AIDS Society (IAS) webinars last week. Despite varied contexts and constraints, the pandemic has highlighted many similarities between countries regarding challenges and successes in HIV service provision.
Challenges with lack of viral suppression, late presenters and new HIV diagnoses
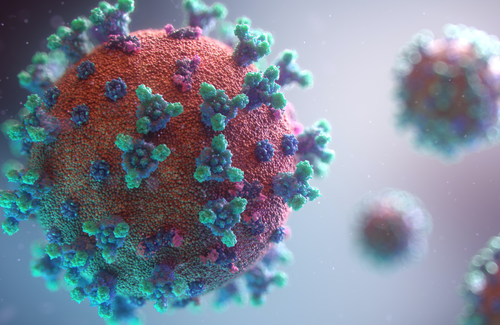
While there is currently limited knowledge about the potential effects of COVID-19 on people with HIV, the healthcare professionals acknowledged that HIV-positive patients on successful antiretroviral therapy (ART) with suppressed HIV would most likely fare better against COVID-19 than those with uncontrolled HIV and weakened immune systems. Currently, it does not appear that those with well-controlled HIV are at a greater risk of contracting the new coronavirus.
However, there are concerns regarding those who are not currently on ART, not virally suppressed and those who are diagnosed at a late stage of infection. Dr Estevão Nunes highlighted the fact that just under 30% of those presenting for treatment with HIV in Brazil still present at a late stage with severely compromised immune systems. This raises concerns over opportunistic infections, such as pneumonia and tuberculosis (TB). Professor Graeme Meintjes from South Africa said that only 54% of those currently on ART in South Africa are virally suppressed. Due to the high rates of current and past TB infection in the country, many are left with post-TB lung damage and disease which may exacerbate the effects of COVID-19.
Concern regarding viral suppression was also echoed by Dr Roberto Paulino-Ramirez from the Dominican Republic, where viral suppression for those on ART is also around the 50% mark. As in many other resource-limited settings, HIV viral load testing is not currently a priority, with the laboratory that previously provided it now dedicated to the new coronavirus.
The pandemic also raises challenges regarding HIV testing services and care for those newly diagnosed with HIV, who require a greater degree of clinical monitoring for both their physical and psychological health. Many clinicians expressed concerns about national lockdowns discouraging people from seeking out HIV testing and follow-up services, with fewer or no face-to-face consultations for sexual health taking place in many settings. There has been a shift to virtual and telephone service provision, with suggestions of the need to scale up HIV self-testing programmes.
Dr Marta Boffito shared the experience of swiftly re-organising London HIV services within a week, with most clinics becoming virtual by offering telephone consultations, leaving only one central London clinic in her organisation open for those who needed to be seen urgently. With many clinicians who were previously devoted to providing HIV and sexual health services redeployed to respond to COVID-19, Dr Monica Gandhi said that HIV services in San Francisco had also moved to telephone consultations. She remarked that it was the first time that individuals with a chronic illness were actively discouraged from seeking out health care and expressed concerns about how those with HIV would be affected by healthcare systems that are overwhelmed by COVID-19.
Maintaining a steady supply of ART
The central challenge for all HIV clinicians has been how to ensure that those currently on ART continue to have an uninterrupted supply of medication and remain adherent despite national lockdowns. Loss to follow-up is already a challenge in many settings and will be further exacerbated by the COVID-19 pandemic. Dr Cristina Mussini from Italy related that fears of contracting coronavirus discouraged some patients from coming to the hospital to collect their ART.
"The central challenge has been how to ensure that those on ART continue to have an uninterrupted supply of medication."
Dr Paulino-Ramirez from the Dominican Republic said that those currently on ART have been given three- to six-month prescriptions and newly diagnosed individuals a month’s prescription. Similar measures have been put in place in many other countries. Dr Ke Liang from Wuhan, China described how doctors themselves delivered supplies of ART to patients in rural areas, while couriers sent medication to others. In some settings, such as in the UK, many living with HIV were already getting their medication via the postal service. There are also concerns about ensuring that those on pre-exposure prophylaxis (PrEP) can maintain access during this time.
In South Africa, the country with the largest ART programme globally (approximately four to five million people on ART), new guidelines suggest that six-monthly supplies of ART are to be given to all clinically stable HIV-positive individuals and that family members should be able to pick up medication. Dr Tracy Flowers, working in the densely populated township of Khayelitsha, said it was important to focus on those who are struggling with adherence and those who are disengaged from treatment. These individuals are even more vulnerable during the current pandemic and would place a greater strain on the healthcare system if they become ill as a result of not taking their ART, so reaching out to them is crucial.
Key populations and gender-based violence
Sex workers, transgender women, people who inject drugs and other key populations are highly marginalised and vulnerable, with lockdown restrictions likely to have more severe effects, said Dr Amira Herdoiza from Ecuador. This was echoed by Dr Catherine Ngugi from Kenya, who explained that sex workers, for example, have high levels of mobility, come into close physical contact with a large number of people, and in many instances are not on ART or not virally suppressed. At the same time, rising levels of gender-based violence during lockdown may affect people living with HIV in vulnerable households.
Opportunities arising from the COVID-19 pandemic
Despite the current challenges, the COVID-19 pandemic may also contribute to finding innovative solutions regarding testing, service delivery and the management of chronic HIV. Dr Herdoiza from Ecuador said that it was important to draw on the lessons learned from the HIV response and apply them to the current pandemic. One is that healthcare workers need to work closely with civil society organisations and communities in order to ensure that solutions are tailored to meet the needs of those affected by HIV and COVID-19.
The pandemic has also opened up new avenues for the care of those who are stable and require fewer clinical interactions, freeing up clinicians to devote more time to those with greater needs. Dr Boffito from the UK ended her talk by saying that upon reflection, the current pandemic might provide important answers to questions about what is next for those living with HIV and what can be done better in future. But that will only be possible after a careful evaluation of what has been missed during this crisis.