
- This page provides a historical overview of major trends in the HIV and AIDS epidemics in the UK from the 1980s to 2020.
- It provides five-year snapshots of key statistics and developments that affected HIV diagnosis, treatment and prevention.
1985
Following reports of the first AIDS cases in the United States in June 1981, the first cases of AIDS in the UK were reported in 1982. Case reports began to increase markedly during 1984 and 1985, with 260 cases reported in 1985 the UK. (Galbraith) Approximately 90% of people diagnosed with AIDS in this period were gay and bisexual men, almost all in London. (McCormick)
By the end of 1985, a test for HIV, the virus that causes AIDS, was available in the UK. Voluntary HIV antibody testing showed that HIV was highly concentrated in three groups: gay and bisexual men, people who inject drugs and people with haemophilia receiving blood products (Factor VIII). Ninety-eight per cent of people diagnosed with HIV to the end of 1985 fell into one of these three exposure categories. (McCormick)
The transmission of HIV through the blood product Factor VIII in the UK was identified in 1984 by the use of experimental antibody tests. (The Penrose Inquiry) Heat-treated Factor VIII, which did not contain HIV, was introduced in the UK in 1985. Prior to its introduction, approximately 1250 people with haemophilia acquired HIV (Infected Blood Inquiry) and 36% of people receiving care at haemophilia treatment centres in the UK had tested HIV positive. (The Penrose Inquiry)

1990
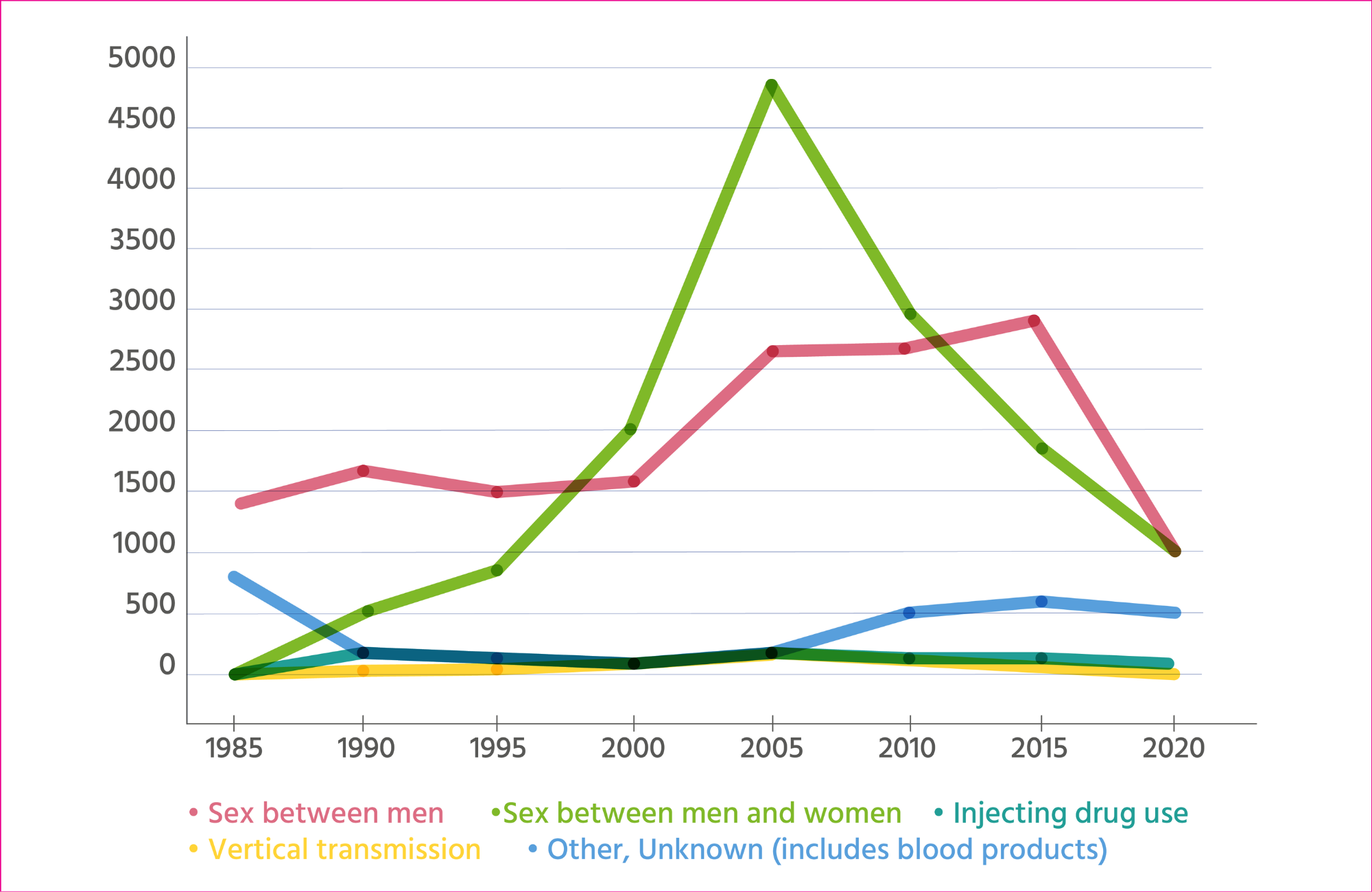
In 1990, 21% of HIV diagnoses were attributed to sex between men and women. (Health Protection Agency Centre for Infections: Quarterly Surveillance Tables) The majority of these cases were reported in people who had lived in or had sexual partners from African countries where the major route of HIV transmission is sex between men and women.
Although government campaigns and many voluntary sector organisations stressed that ‘AIDS affects everyone’ during the late 1980s, 67% of those diagnosed with HIV and 73% of people diagnosed with AIDS were gay or bisexual men in 1990. (Health Protection Agency Centre for Infections: Quarterly Surveillance Tables) The campaigning organisation Gay Men Fighting AIDS was founded in 1992 to restore a focus on HIV prevention for gay and bisexual men in the UK.
The spread of HIV by sharing of injecting equipment began in the UK around 1982 but the scale of transmission was not recognised until HIV antibody testing of people who inject drugs took place in Edinburgh in 1985. (Robertson) HIV prevalence peaked in people who inject drugs in 1990 at just under 6% and fell rapidly after 1990 due to the success of needle and syringe exchange programmes in preventing HIV transmission by sharing of injecting of equipment. (Hope)
1995
No effective treatment to prevent AIDS was available in the period before 1996. 1994 saw the peak of AIDS deaths and diagnoses in the UK, with 1531 people dying of AIDS and 1851 people diagnosed with AIDS in the UK. (Health Protection Agency Centre for Infections: Quarterly Surveillance Tables)
By 1995, HIV in women and children had been recognised as a significant feature of the UK epidemic. HIV prevalence in mothers in London was almost six times higher in 1993 compared to 1988. (Nicoll) By 1996, 797 children had been diagnosed with HIV in the UK, including 128 diagnosed with AIDS.
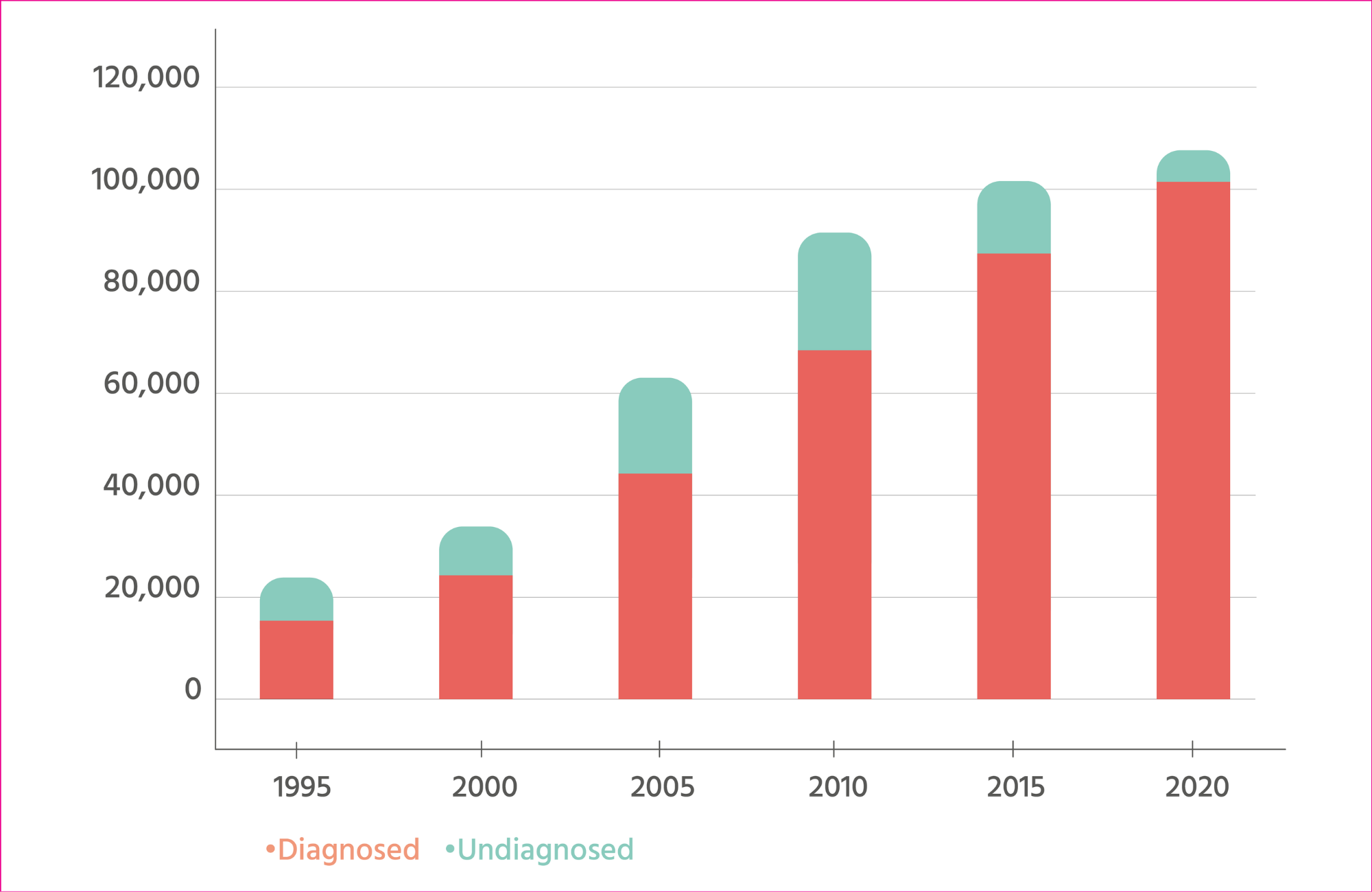
Estimates of the total number of people living with HIV – including people who had never taken an HIV test – began to be produced and refined in the 1990s. It was thought that at the end of 1994, there were 23,000 people living with HIV in the UK, including 7500 (36%) who had not been diagnosed. (Allardice)
2000
In 1996, highly active antiretroviral therapy (HAART) consisting of three-drug combinations was introduced. HAART restored the immune system and stopped the development of AIDS. Deaths from AIDS fell by 80% between 1995 and 2000, from 1514 to 295. New AIDS diagnoses fell by half between 1995 and 2000.
As a result, the number of people living with HIV began to rise substantially. HIV diagnoses also increased, reflecting an increase in HIV testing, ongoing HIV transmission among gay and bisexual men and a large increase in HIV diagnoses in men and women with heterosexually acquired HIV. (Rice)
HAART had little impact on HIV transmission during this period because not enough people with HIV were taking it to stop transmission on a large scale.
2005
HIV diagnoses peaked in 2005 (7697 cases). The period between 2000 and 2005 was the peak period of HIV diagnosis among heterosexual men and women (4822 in 2005) and the peak period of HIV diagnosis in women (3261 in 2005). The increase in HIV diagnoses in women coincided with the introduction of opt-out antenatal testing for HIV from 1999.
The increase in diagnoses of heterosexually acquired HIV up to 2005 reflects migration from countries in Africa with high HIV prevalence. HIV diagnoses reached their highest level among Black Africans in the UK in 2003, when 3976 Black Africans were diagnosed with HIV.
There were 2660 HIV diagnoses in gay and bisexual men, which is over 1000 more cases than five years earlier. The increase was largely a consequence of an increase in HIV testing; 47% of gay and bisexual men received an HIV test when attending a sexual health clinic in 1998, compared to 79% in 2004. (Health Protection Agency Centre for Infections: Mapping the Issues)
2010
There were an estimated 91,500 people living with HIV in the UK in 2010, almost three times as many as a decade earlier. However, one in four (24%) remained undiagnosed.
The number of people accessing HIV care grew from 22,600 in 2000 to 69,400 in 2010 due to increased HIV testing and improved life expectancy for people with HIV. (Health Protection Agency) By 2010, antiretroviral treatment was easier to take (one tablet a day) and had fewer side effects.
2015
This period saw a big increase in the number of people taking antiretroviral treatment in the UK, increasing from 56,100 people in 2010 (Health Protection Agency) to 83,931 in 2015. (Public Health England, 2016) In 2012, the British HIV Association (BHIVA) recommended that anyone who wanted to start HIV treatment to avoid transmitting HIV should be able to do so. In 2015, BHIVA recommended that everyone with HIV should start treatment as soon as possible after diagnosis.
The period between 2010 and 2015 saw a 50% reduction in AIDS diagnoses (662 cases in 2010 to 305 in 2015) as people with HIV were diagnosed earlier and started treatment sooner. In 2015, approximately 13% of people with HIV remained undiagnosed, compared with 24% in 2010. (Public Health England, 2016) (Health Protection Agency)
Just over 6000 people a year were diagnosed with HIV between 2010 and 2015, one of the highest rates of diagnosis in western Europe. Each year between 2006 and 2015, more than half of people diagnosed with HIV in the UK were born abroad. (Public Health England, 2016)
By 2015, HIV diagnoses in women were 60% lower compared to 2005. (Public Health England, 2016)
2020
Between 2015 and 2020, substantial falls in HIV diagnoses occurred in all groups due to the impact of antiretroviral treatment on HIV transmission. In 2017, the UK reached the UNAIDS target of 90% of people with HIV diagnosed, 90% of diagnosed people on antiretroviral treatment and 90% of people on treatment being virally suppressed. (Public Health England, 2018)
In gay and bisexual men, new HIV diagnoses fell by two-thirds between 2015 and 2020 due to the combined impact of treatment as prevention and pre-exposure prophylaxis, or PrEP, the use of antiretroviral drugs by HIV-negative people to prevent HIV acquisition. (UK Health Security Agency) PrEP became available through the PrEP Impact trial in England and on an unlimited basis in Scotland and Wales from 2017.
Cases of AIDS continued to decline (178 in 2020) and relatively few deaths were due to AIDS. In 2020, the leading causes of death in people with HIV were COVID-19 (25%), cancers (20%), AIDS-defining conditions (12%), cardiovascular disease (11%) and substance use (6%). (Croxford)
By 2020, just under 5% of people with HIV were unaware of their HIV status. (UK Health Security Agency)
Note
Data in the graphs comes from the Public Health Laboratory Service, Health Protection Agency and UK Health Security Agency.
Galbraith NS et al. The acquired immune deficiency syndrome—1985. Community Medicine, 8: 329-36, 1986.
McCormick A et al. Surveillance of AIDS in the United Kingdom. British Medical Journal, 295: 1466-69, 1987.
The Penrose Inquiry. Final Report. Volume 2. Chapter 10, Section 10.13. 2015.
Infected Blood Inquiry. Expert Report to the Infected Blood Inquiry: Statistics. September 2022.
The Penrose Inquiry. Final Report. Volume 2. Chapter 10, Table 10.1. 2015.
Health Protection Agency Centre for Infections. AIDS/HIV QUARTERLY SURVEILLANCE TABLES no 69, 2005.
Robertson R. Misadventure in Muirhouse. HIV infection: a modern plague and persisting public health problem. Journal of the Royal College of Physicians of Edinburgh, 47: 88-93, 2017.
Hope VD et al. Two decades of successes and failures in controlling the transmission of HIV through injecting drug use in England and Wales, 1990 to 2011. Eurosurveillance, 19: 20762, 2014.
Nicoll A et al. Epidemiology and detection of HIV-1 among pregnant women in the United Kingdom: Results from national surveillance 1988-96. British Medical Journal, 316: 253-8, 1998.
Allardice G & Hughes G. AIDS and severe HIV disease: combined predictions for the United Kingdom to 1999. Communicable Disease Report, 6: R192-4, 1996.
Rice BD et al. Prevalent diagnosed HIV in England, Wales and Northern Ireland, adjusted totals 1996-2001 and extrapolations to 2004. AIDS, 18: 927-32, 2004.
Health Protection Agency Centre for Infections. Mapping the Issues. HIV and other Sexually Transmitted Infections in the United Kingdom: 2005. 2005.
Health Protection Agency. HIV in the United Kingdom: 2011 report. November 2011.
Public Health England. HIV in the United Kingdom: 2016 report. December 2016.
Public Health England. Progress towards ending the HIV epidemic in the UK: 2018 report. November 2018.
UK Health Security Agency. HIV testing, new HIV diagnoses, outcomes and quality of care for people accessing HIV services: 2021 report. 2021.
Croxford S et al. Mortality among people with HIV in the UK in 2020: findings from the National HIV Mortality Review. British HIV Association Spring Conference 2022, Manchester, abstract no O06.
