A qualitative study sought to understand healthcare workers’ perspectives on patients who disengage from antiretroviral therapy (ART) at a clinic in Cape Town, South Africa. Results, presented this week to the 11th International AIDS Society Conference on HIV Science (IAS 2021) showed that healthcare workers had contradictory feelings about these patients, ranging from empathy to anger.
Having sub-optimal adherence to or stopping HIV treatment can lead to drug resistance, HIV transmission, poor health outcomes, and higher cost of care. Research has shown that negative attitudes and punitive or paternalistic treatment from healthcare workers negatively impacts adherence to HIV treatment. However, previous studies haven’t focused on the perspectives of healthcare workers or their understanding of HIV care disengagement.
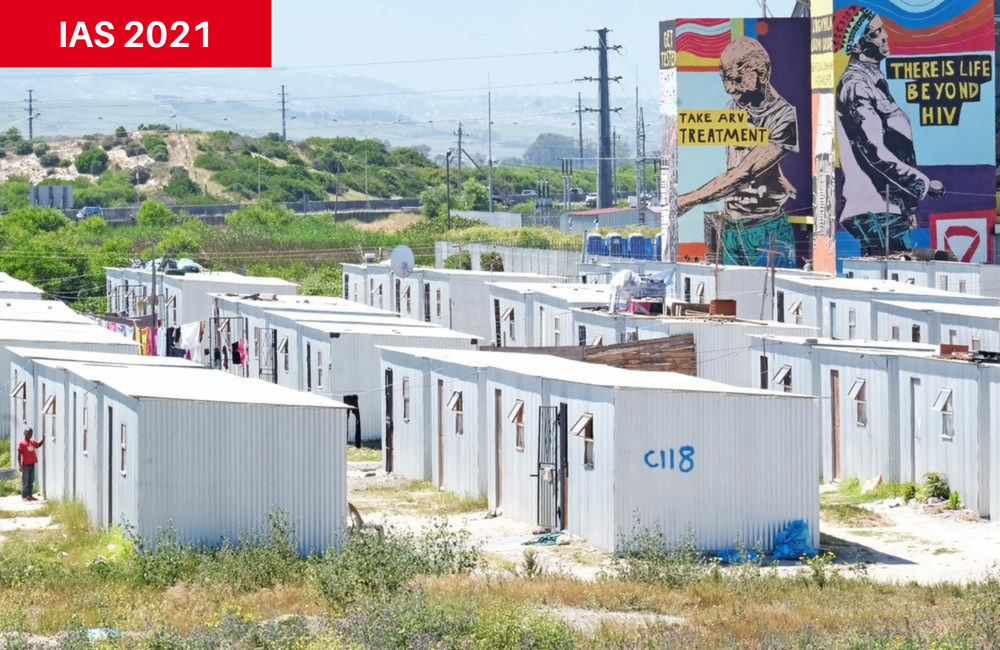
Led by Tsephiso Nhemachena of the University of Cape Town and in collaboration with Médecins Sans Frontières, researchers conducted semi-structured interviews with 30 doctors, nurses, counsellors, social workers, data clerks, security guards, and allied health professionals at a primary healthcare clinic in Khayelitsha, Cape Town, South Africa.
Eligible participants were aged 18 and older and had worked at the clinic at least one year. They also interacted with patients participating in the ‘Welcome Service’ – a pilot programme designed to support retention among patients returning to HIV care after an interruption.
During the interviews, healthcare workers were asked to give examples of patients who interrupt treatment and how they feel when dealing with a patient who is returning to care. They were also asked about reasons why patients disengage from treatment and whether the healthcare worker thought they were reasonable.
The first theme that emerged from the interviews was that disengagement was a threat to individual and public health and deserved attention. One participant stated that:
“It is a problem because like you know, like the virus becomes resistant to medication, so which is posing danger to the person who is not taking the medication you know”.
Empathy for patients was the second theme. Participants mentioned that disengagement was often due to factors outside a patient’s control, such as mental health challenges, and discussed how non-disclosure of HIV status presents a barrier. The healthcare workers expressed concern for their patients:
“I get worried and concerned. I want to know the reasons so that we can tackle whatever challenges she has to overcome those challenges so that the patient can be able to take treatment”.
In contrast, the final theme identified was anger. This stemmed from increased workloads from the high medical and psychosocial needs of patients who disengaged from care, as well as a belief that patients weren’t prioritising their health. Healthcare workers expressed frustration that their patients would discontinue life-saving treatment:
“...for example why didn’t you take your ARV’s; I don’t have any reason. Now you’re like, well you just... I just want to strangle her... because I don’t understand, I don’t understand how come the person will just disengage their treatment for no reason”.
As gatekeepers to HIV care, healthcare workers play an important role in HIV treatment adherence and care engagement. In this study, the healthcare workers had conflicting feelings about patients who disengage from care, ranging from empathy to anger. Negative attitudes from healthcare workers are barriers to care and can perpetuate disengagement.
The Welcome Service intervention was developed to support retention in care. The programme included training, support, and mentoring for healthcare workers to address negative attitudes and beliefs towards people living with HIV who had disengaged from care. Services were reorganised so as to reduce delays in HIV treatment reinitiation, shorten waiting times and prioritise sick clients. Patients were offered psychosocial support and counselling to address specific barriers to care.
The intervention has had modest results. Sixty per cent of clients enrolled were retained in care at one year, around half of clients enrolled completed a viral load test at one year, and about half of those receiving a viral load test were virally suppressed. High staff turnover was a barrier, and the researchers noted that addressing healthcare workers’ stigmatising attitudes was challenging and required constant re-engagement.
The authors call for more interventions, training, and support to help healthcare workers navigate the contradictory feelings that can arise from working with patients who disengage from HIV treatment.
Nhemachena T et al. Between empathy and anger: Healthcare workers' perspectives on patient disengagement from antiretroviral treatment in Khayelitsha, Cape Town. 11th IAS Conference on HIV Science, abstract OAD0701, 2021.
Arendse, K. Addressing disengagement from HIV healthcare services in Khayelitsha, South Africa, through Médecins Sans Frontières' Welcome Service approach: comprehensive clinical and patient-centered care. 11th IAS Conference on HIV Science, abstract PED448, 2021.
