Once someone is infected with HIV the virus usually persists in their body and HIV infection is lifelong.
This does not mean they will get sick. These days, if people are diagnosed promptly and start taking antiretroviral therapy (ART) before HIV has caused damage to their immune system, they are unlikely ever to suffer from one of the HIV-related illnesses collectively known as AIDS and can have a normal life expectancy.
Even if people are diagnosed late and are unwell due to HIV-related immune deficiency, immediate ART usually prevents disease progression and death.
But this is not the same as a cure for HIV. Antiretroviral drugs block HIV’s lifecycle. They stop it replicating (copying itself) and causing immune damage. But if someone stops taking ART or does not take it consistently, then HIV can start replicating again.
Many viral infections, like colds, COVID and hepatitis A, are usually self-limiting. This means that the body’s natural defence system (the immune system) contains the illness by itself and, sooner or later, eliminates the infection, unless there are underlying problems. But certain other viruses hide away in locations in the body where the immune system cannot detect or eliminate them. Herpes and hepatitis B can persist in this way.
But they do not penetrate the inner sanctum of cells – the nucleus, which contains the genes. In the case of HIV, it inserts its viral genes – the ‘instructions’ for making new viruses – into the host genes of certain long-lived immune cells, as lengths of so-called ‘proviral’ DNA. Here they are invisible to the immune system. These cells are, in the main, central memory T-cells, whose job is to remember and react to previous infections. They are often termed the HIV reservoir. If ART is stopped, these cells act as the source for a new burst of viral infection. That is why HIV infection is lifelong.
Despite this, we know HIV infection can be cured. But so far, cures have only been confirmed in a handful of cases.
There are two main ways HIV cures have been achieved.
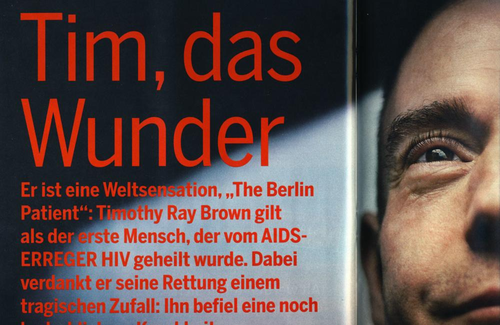
Five people have now been cured of HIV by advanced medical techniques. These have involved replacing all the cells in their immune systems with ones from donors that are resistant to HIV. In these people every trace of HIV appears to have been eliminated from their system. Their cells may still contain fragments of HIV genetic material, but none that is ‘viable’ – entire enough to give rise to new virus.
A sixth person has been cured by a similar immune transplant, except that in his case the new cells were not naturally resistant to HIV. Despite this he shows all the signs of HIV being eliminated from his system and has been off ART without any sign of HIV reappearing for almost two years. Research is ongoing to find out how this happened.
These complete immune-system transplants are expensive, often don’t work, and pose considerable health risks in themselves. They have therefore, so far, only been performed on people who need such transplants for life-threatening cancers of the immune system, such as leukaemia or lymphoma. So a lot of cure research focuses on ways of eradicating someone’s HIV-infected cells in ways that are simpler and less toxic.
The second kind of cure has occurred in some people whose own immune systems appear to have eliminated all, or nearly all, the HIV-infected cells in their bodies, or at least keep HIV’s activity contained at such a low level that it does no harm.
In some cases, people seem to have unusually strong responses to HIV from the start. These responses keep it controlled and eventually eliminate it, without ever needing to take ART. In some cases, they have acquired naturally weak strains of the virus or have cells naturally more resistant to infection. In other cases, they may have unusually strong and specific immune reactions to HIV. These people are often termed ‘elite controllers’, meaning they can preserve their normal immune function and maintain an undetectable HIV viral load without the need of drugs. A few of these people, however, have no unimpaired HIV left and have been termed ‘exceptional elite controllers’.
Other people with strong immune responses – especially, but not entirely, people treated very soon after infection – have a more typical early course of HIV infection and start antiretroviral therapy (ART). But the ART seems to suppress the amount and activity of HIV in their body to such an extent that their own immune responses can sufficiently control the little bit that is left when they stop taking ART. They are sometimes termed ‘post-treatment controllers’.
Another major focus of cure research is how some people control HIV without treatment, and developing therapies to help more people do the same thing.
Many people living with HIV hope for a cure which completely clears all traces of viable HIV from the body, as has been achieved for a few people following replacement of immune system cells with a stem cell transplant. This can be called a ‘complete cure’, ‘eradication’ or ‘elimination’. This is sometimes also referred to as a ‘sterilising cure’, although that term has unpleasant connotations for many.
However, such a complete cure may be difficult to achieve. Even if there is one, it’s hard to prove that there are no cells containing HIV left in the body. The situation may therefore be described as a ‘functional cure’, ‘long-term control off therapy’, or ‘remission’. The latter is a term borrowed from cancer therapy, in which remission may be reported as the length of time someone has been off therapy without disease reappearing. Some cases of apparent cure may be cautiously described as ‘remission’ before there is more definitive evidence of cure. Sometimes a remission may become so deep and last so long that it becomes equivalent to an elimination.