A programme to encourage clinicians to switch people to generic antiretroviral drugs saved the NHS almost £10 million in the financial year 2016-2017, Dr Laura Waters of NHS England’s Clinical Reference Group for HIV services told the recent joint British HIV Association (BHIVA) and British Association for Sexual Health and HIV (BASHH) conference in Edinburgh.
However, the switch to new tablets has not been smooth for all patients, with several HIV clinics reporting a higher than expected number of people who did not make the expected switch or needed to go back to their original therapy after switching.
Around two-thirds of NHS England’s spending on HIV medical care is for antiretroviral drugs, with £429 million spent in 2015-2016. Because of the increasing number of people needing lifelong treatment, the drugs budget would continue to grow if action were not taken.
Across the NHS, around 70% of drugs prescribed are produced by generic manufacturers. As the patents of many anti-HIV drugs have now expired, generic versions of these drugs are now available. They have the same active ingredients as branded drugs but are cheaper.
Savings can also be made by switching people from protease inhibitors boosted with ritonavir to protease inhibitors boosted with cobicistat. The latter are now cheaper and are also available in fixed-dose combinations, therefore reducing pill burden. Although ritonavir and cobicistat perform similar functions, this is not a ‘like for like’ switch.
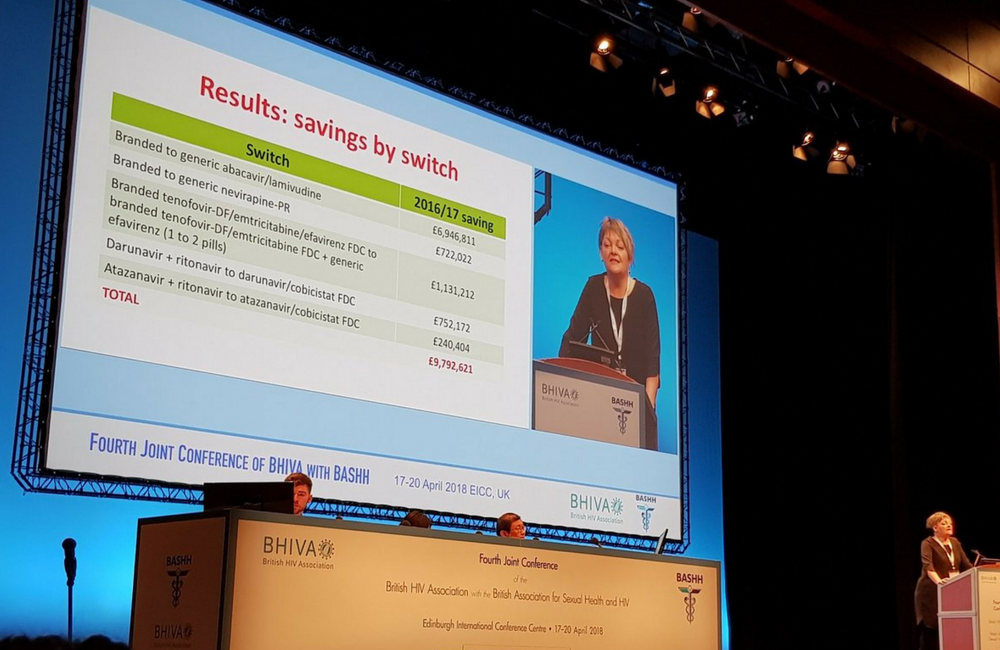
The HIV Clinical Reference Group identified a 'menu' of recommended changes of antiretroviral treatment. While making cost savings was one objective, Waters stressed that this was a programme driven by doctors and patient representatives, in which only clinically appropriate and acceptable switches were recommended. They were:
- Switching from branded abacavir/lamivudine (Kivexa) to a generic equivalent, with no change of pill burden
- Switching from prolonged-release nevirapine (Viramune) to a generic equivalent, with no change of pill burden
- Switching from branded efavirenz/tenofovir DF/emtricitabine (Atripla) to generic efavirenz + branded tenofovir DF/emtricitabine (Truvada), an increase from one pill to two
- Switching from darunavir (Prezista) + ritonavir (Norvir) to darunavir/cobicistat (Rezolsta), a decrease from two pills to one
- Switching from atazanavir (Reyataz) + ritonavir (Norvir) to atazanavir/cobicistat (Evotaz), a decrease from two pills to one.
Although these changes were not fully rolled out in all regions in 2015-2016, almost £10 million was saved in that year, with the greatest savings coming from abacavir/lamivudine (£6,947,000). The efavirenz switch also saved a considerable amount (£1,131,000).
The overall antiretroviral drug budget for NHS England in 2015-2016 was £414 million. This was 3.6% lower than in the previous year, more than the targeted saving of 2.5%. Two-thirds of the savings came from these switches and a third from renegotiating contracts with pharmaceutical companies, who were under pressure to lower prices. For example, the manufacturer of dolutegravir/abacavir/lamivudine (Triumeq) reduced its price to avoid people being switched away from it.
Implementation challenges
However, individual clinics reported some challenges with implementing these switches. At the Chelsea & Westminster Hospital in London, 1556 of 2547 patients (61%) taking Atripla switched to generic efavirenz + branded tenofovir DF/emtricitabine (Truvada), as planned. However, 648 (25%) switched to a different combination that did not contain efavirenz.
When asked to consider the switch, many people used this as an opportunity to review their treatment as a whole. Although many people had previously put up with low-level, long-term side-effects of efavirenz, there’s now more awareness that alternate drugs are available and that efavirenz is no longer a first-line choice for treatment.
When people switched to a different treatment, the most popular choices were raltegravir (Isentress) + tenofovir DF/emtricitabine (Truvada), dolutegravir/abacavir/lamivudine (Triumeq) and rilpivirine/ tenofovir DF/emtricitabine (Eviplera).
In addition, 97 of 1604 (6%) of those who switched to generic efavirenz subsequently stopped taking it, usually because of side-effects such as problems sleeping, vivid dreams, depression, dizziness, problems concentrating and headache. As a result of permitted variations in quantities of a drug’s active ingredient and manufacturing differences, some people have different experiences of side-effects when taking different versions of the same drug.
Similarly, clinicians at Barts Health said that of 608 people who were switched to darunavir/cobicistat (Rezolsta) and 193 people switched to atazanavir/cobicistat (Evotaz), 81 patients (10%) subsequently needed to change their treatment, most often switching back to their previous combination.
In over half the cases, the problem was greater side-effects (especially diarrhoea, other gastrointestinal problems and problems sleeping) or a deterioration of kidney function. The size of the new tablet was also an issue for some people and seven needed to switch because of treatment failure or drug resistance.
These issues affect a minority of people asked to switch, but do they result in extra spending that negates the cost savings that were hoped for? Extra clinic visits, extra tests and drug wastage could be ‘hidden costs’ that need to be taken into account.
The Manchester Centre for Sexual Health at the Hathersage Centre found that 29 of the 432 people (6.7%) who switched treatment required a further treatment switch. In the first six months, these switches were associated with an extra £45,000 of spending which must be set against the £154,000 that would otherwise be saved.
A limitation of this analysis was that costs were calculated only for the first six months, when the extra costs of people having difficulties with a treatment switch are most likely to be incurred. When people switch and there are no problems, this is likely to result in cost savings over a much longer period. But even with this short time frame, the Manchester analysis found that switching did save money.
Waters L et al. Was the pain worth the gain? Antiretroviral (ARV) savings from the Improving Value project and generics use in England. Abstract O1.
Update: Following the conference presentation, this study was published in a peer-reviewed journal:
Waters L et al. Was the pain worth the gain? Antiretroviral savings from the ‘Improving value’ project and generics use in England. Clinical Medicine, 19: 76, March 2019.
Tyler P et al. A review of switching people living with HIV (PLWH) from Atripla to Truvada and generic efavirenz (gEFV). Abstract P2.
Byrne L et al. Why do people switch away from cobicistat-boosted protease inhibitors? Abstract P34.
Okecha E et al. NHS England commissioning for value:whatis the hidden cost? Abstract O2.
All presentations are from the Fourth Joint Conference of the British HIV Association (BHIVA) with the British Association for Sexual Health and HIV (BASHH), Edinburgh, April 2018.

